This article was written by Jennifer Mueller, JD. Jennifer Mueller is an in-house legal expert at wikiHow. Jennifer reviews, fact-checks, and evaluates wikiHow's legal content to ensure thoroughness and accuracy. She received her JD from Indiana University Maurer School of Law in 2006.
There are 19 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 10,204 times.
There are five levels of Medicare appeals for Medicare Parts A and B (original Medicare). Begin with an initial request to your plan for a redetermination. If you are unhappy with the result, then you can continue to appeal all the way up to a federal district court. To bring a successful appeal, you should gather supporting documentation and seek any assistance provided by a doctor or advocate. The process for appealing a Medicare Prescription Drug Plan is somewhat different at the start of the appeals process.
Steps
Requesting Redetermination (Appeal Level 1)
-
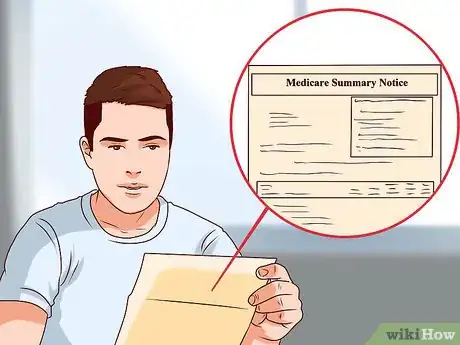
1Read your Medicare Summary Notice. Every three months you should receive a summary of the services and supplies that were billed to Medicare during the timeframe. You will also see whether or not Medicare agreed to cover payment fully or partially.
- Look over your Medicare Summary Notice when it arrives and note if there is something Medicare has chosen not to reimburse. Each Medicare Summary Notice should inform you of how you can appeal.[1]
-
2Decide if you need a fast-track appeal. You have a right to a decision in 72 hours if you think waiting would seriously harm your health.[2] If you want to fast-track an appeal, then speak to your doctor.Advertisement
-
3Get assistance. You can get help bringing a Medicare appeal. For example, you can contact your State Health Insurance Assistance Program (SHIP). These agencies provide in-depth counseling to Medicare beneficiaries.[3] You can find your state SHIP by using the SHIP locator tool at the State Health Insurance Assistance Program National Technical Assistance Center’s website (www.shiptacenter.org).
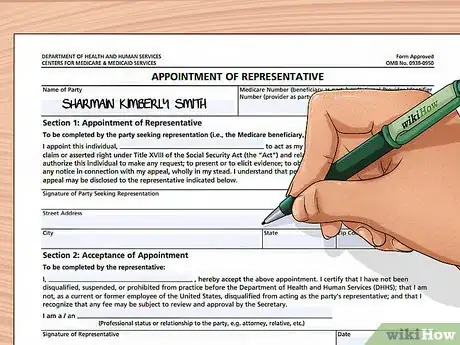
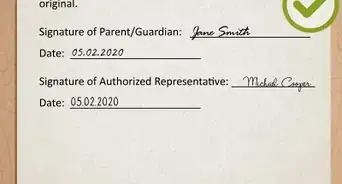
- You might also want to appoint someone as a representative. This representative will be authorized to file appeals on your behalf. Various people can serve as representatives. For example, a friend, family member, lawyer, doctor, or other person can serve as a representative.[4]
- To appoint a representative, you should complete the “Appointment of Representative” form, available for download at https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/downloads/cms1696.pdf.
- You can also appoint a representative by writing a letter. Make sure the letter contains the following information:
- your name and contact information
- your Medicare number
- a statement in which you appoint someone as your representative
- the name and contact information of the representative
- the representative’s relationship to you and professional status (e.g., a doctor)
- a statement authorizing the release of personal and identifiable health information to the representative
- a statement explaining why and to what extent you are being represented
- your signature and date
- the representative’s signature and the date
-
4Gather documents. You should contact your doctor and gather any materials that will help you with your appeal.[5] You should provide copies (not originals) of these documents with each appeal form that you submit.
- Talk to your doctor about what information would help bolster the strength of your appeal. For example, Medicare might not believe that certain treatments or services are medically necessary. Your doctor can help you gather evidence to show that the services are in fact necessary.
-
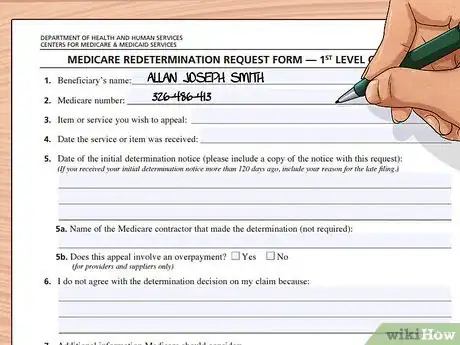
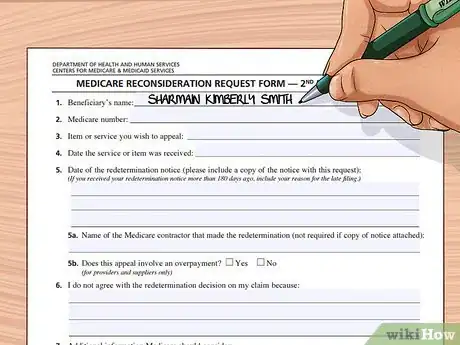
5Complete a “Redetermination Request Form.” You can download this form at https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/downloads/CMS20027.pdf. You can type information into the PDF or you can print off the form and neatly write in the information.
- You will then mail it to the address provided on your Medicare Summary Notice.[6] Be sure to keep a copy for your records.
-
6Write a letter. If you do not want to submit a Redetermination Request Form, then you can send a written request. Be sure that it contains the following information:[7]
- your name and Medicare number
- the items/services you are appealing and the dates of those services
- your reasons why you disagree with the initial determination
- your signature or the signature of an appointed representative
-
7Receive your Medicare Redetermination Notice. After you submit your appeal and all supporting documentation, you will receive a decision within 60 days. You will receive a Medicare Redetermination Notice in the mail.[8]
- If you disagree with the determination, you may appeal to the next level.
Requesting Reconsideration (Appeal Level 2)
-
1Fill out a request form. You can request reconsideration by filling out a “Medicare Reconsideration Request Form” and mailing it to a Qualified Independent Contractor (QIC). QICs are private companies that contract with Medicare to handle appeals. They are not involved in the initial redetermination. To request reconsideration, you can download the applicable form at https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/downloads/cms20033.pdf.
- You can type your information into the PDF or print off the PDF and type or write the information on the form. Make sure your information is legible.
-
2Write a letter. If you do not want to use the form, you can write a letter and submit it. You should make sure to include the following information in the letter:[9]
- your name and Medicare number
- the services or items you are requesting to be reconsidered
- the date of the services
- the company that made the redetermination (look at your Summary Notice)
- your reason why you disagree with the redetermination decision
- your signature (or the signature of an appointed representative)
-
3Mail the form or letter. Send your request to the QIC listed on the Redetermination Notice.[10] Be sure to send it certified mail, return receipt requested so that you will know that it has been received. Keep a copy of the appeal form for your records.
-
4Receive written notice. About 60 days after you mail your appeal form, you should receive a “Medicare Reconsideration Notice.” If you want to appeal the determination, then you have 60 days to do so.[11]
- Furthermore, if the QIC takes more than 60 days to issue a decision, you may request that it forward your appeal to an Administrative Law Judge, which is the third level of appeal.
Getting a Hearing before a Law Judge (Appeal Level 3)
-
1Check if you qualify. In order to be able to appeal to this level, your appeal must have a dollar amount of at least $160. You may be able to combine claims to reach this threshold.[12]
-
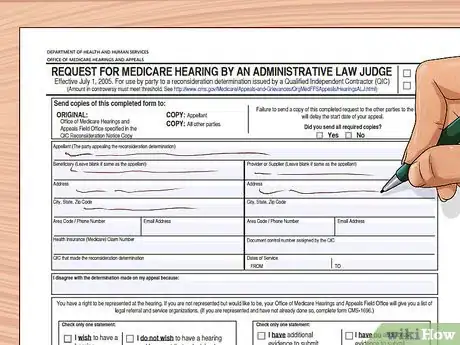
2Make the request. You have 60 days after receiving your “Medicare Reconsideration Notice” to request a hearing before an Administrative Law Judge (ALJ). You can make the request by filling out the “Request for Medicare Hearing by an Administrative Law Judge” form, which is available at https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/downloads/cms20034ab.pdf.
-
3Write a letter instead. If you do not want to complete the form, then you can write a letter. The letter must contain the following information in order to be effective:[13]
- your name, address, and Medicare number
- the name of a designated representative
- the document control number (if any) assigned by the QIC
- the dates of service that you are appealing
- why you disagree with the QIC’s decision
- a statement describing any additional evidence you will submit and when you will submit it
-
4Mail the request. Send it to the address specified in your Notice of Reconsideration. In most situations, you will mail it to HHS OMHA Centralized Docketing, 200 Public Square, Suite 1260, Cleveland, OH 44114-2316.[14]
-
5Receive your Notice of Hearing. After receiving your application, the ALJ reviews the claim and then sets up the hearing. You will be sent a Notice of Hearing informing you of the date, time, and location of the hearing. You will receive it at least 20 days before the scheduled hearing.[15]
-
6Complete your Response form. After receiving the Notice of Hearing, you have to fill out and submit a Response to Notice of Hearing Form and return it to the ALJ. The form should be mailed to you.[16]
-
7Select your hearing site. Most hearings will be conducted by videoconferencing. With videoconferencing, you and the ALJ will be able to see and hear each other. You will participate in the video conference by going to a private room. The technician will make sure the equipment is working. You will be able to select the videoconferencing site nearest to you.[17]
- You can request an in-person hearing with the ALJ instead, but you must have reasons for requesting one.[18]
-
8Attend the hearing. At the hearing, the ALJ will summarize the issues and may ask you questions. If you have witnesses that support your case, then they should come with you to the video conference room. The judge will want to ask any witnesses questions.
- All witnesses will testify under oath. An audio recording will also be made.[19]
- Remember to speak clearly and think before speaking. Always tell the truth. If you need to take a break, then politely ask the judge if you can take a break.
-
9Receive a written decision. In most cases, the ALJ will mail you a written decision within 90 days. If you disagree with the ALJ’s decision, then you have 60 days to file an appeal.
- If the ALJ doesn’t issue a timely decision, then you can request that your case be forwarded to the Medicare Appeals Council, which is the fourth level of appeals.[20]
Appealing to the Medicare Appeals Council (Appeal Level 4)
-
1Read your hearing decision. The decision the ALJ sends to you will contain important information about your appeal to the Medicare Appeals Council. For example, the ALJ’s decision should tell you who to contact for your appeal.
-
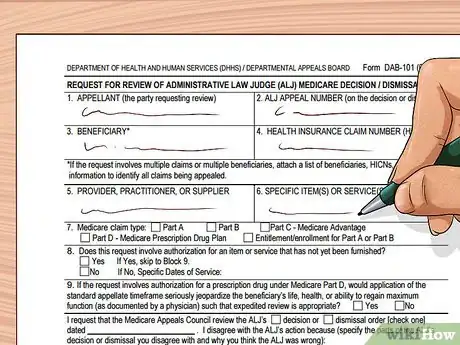
2Complete a form. You can request an appeal from the Appeals Council by completing a “Request for Review of an Administrative Law Judge (ALJ) Medicare Decision/Dismissal” form. It is available for download at http://www.hhs.gov/dab/divisions/dab101.pdf.
- You will need to print this form off and type in or write the information.
- You will also need to attach a copy of the ALJ decision or dismissal order.[21] Be sure to make a copy but keep the original for your records.
-
3Write a letter. If you don’t want to use the form provided, then you can also write a letter. Make sure to include the following required information:[22]
- your name and Medicare number
- the items or services you are appealing, including the dates of those services (see your ALJ decision)
- a statement in which you identify the parts of the administrative law judge's decision that you disagree with, including the reasons why you disagree
- the date of the ALJ’s decision
- your signature or your appointed representative's signature
- the ALJ hearing office (if the ALJ has not issued a timely decision)
-
4Call with questions. If you have questions, then you should call the Medicare Appeals Council staff at (202) 565-0100.[23] Make note of when you call and who you spoke to. Also summarize the conversation as best as you can.
-
5Mail the form/letter. You should mail the letter to the address provided in the ALJ’s decision. You may also fax your appeal request to (202) 565-0227. If you send the request by fax, then you do not need to mail a copy.[24]
- Keep a copy for your records.
-
6Receive a written decision. Typically, the Appeals Council will send a written decision within 90 days of receiving your request. If you disagree with the decision, then you can seek an appeal to a federal district court, which is the fifth level of appeals.[25]
- If the Appeals Council takes too long, then you can ask the Council to forward your case to the next level.
Requesting Judicial Review in Federal District Court (Appeal Level 5)
-
1Satisfy the minimum dollar amount. In order to seek judicial review in federal district court, your claim must be worth at least $1,600 ($1,630 for 2019). You might be able to combine claims to meet this amount.[26]
-
2Read your Appeals Council decision. The decision should give you directions about how to appeal in federal district court.[27]
-
3Meet with an attorney. Once you decide to follow an appeal all the way up to the federal district court, you will now need professional legal assistance. The rules of federal court are complicated. Furthermore, your claim may be worth a substantial amount of money. You don’t want to lose at federal district court because you don’t understand the court procedures.
- You should find an experienced health care or Medicare attorney by visiting your state’s bar association. This association should either run a referral program or have information for how to get a referral.
-
4File a complaint. You will initiate a lawsuit by filing a complaint with the federal court. You should let your lawyer handle this. Be aware that litigation in the federal courts is extremely slow.
- For more information, see File a Federal Lawsuit.
Bringing a Medicare Prescription Drug Appeal
-
1Talk to your doctor. Appealing the denial from your Medicare prescription drug plan is similar to appealing an “original Medicare” decision. However, you initially need to start by talking to your doctor. Ask if there are any generic, over-the-counter medicines that you could take instead of the medication Medicare refuses to pay for.[28]
-
2Ask for a coverage determination. You or your doctor needs to contact your prescription drug plan. Ask for a coverage determination. If you haven’t yet bought the drugs, then you can make the request by calling the plan on the phone.[29]
- If you have already bought the drugs and want reimbursement, then you must complete a “Request for Medicare Prescription Drug Coverage Determination” form, which is available for download at https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovGenIn/downloads/ModelCoverageDeterminationRequestForm.pdf. Fill it out and mail it to the address provided. Keep a copy for your records.
-
3Receive a determination. The plan has 72 hours to notify you of its decision. If you need an expedited determination, then have your doctor call and explain why not receiving the drug could jeopardize your health. You will receive an expedited determination in 24 hours.
-
4Request Redetermination. If you are unhappy with your plan’s decision, then you can proceed to a Redetermination. You should follow the directions in your plan’s initial denial notice. You have 60 days to appeal.
- You can request Redetermination over the phone or in writing. If you need an expedited decision, explain the reasons. The plan will review your request and issue a written “Redetermination Notice” either within 72 hours (for an expedited request) or within 7 days (if a standard request).
-
5Request Reconsideration by an Independent Review Entity (IRE). After receiving your “Redetermination Notice,” you have 60 days to appeal to an IRE.[30] You should read the Redetermination Notice and follow the instructions.[31]
- You should be sent a “Request for Reconsideration” form which you can use.[32]
-
6Continue your appeals. If the IRE rules against you, then you can continue to appeal, using the same process as appeals for original Medicare (described above). The process will be the following:[33]
- Level 3: appeal to an administrative law judge (ALJ)
- Level 4: appeal to the Medicare Appeals Council
- Level 5: appeal to a federal district court
References
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/filing-an-appeal-if-i-have-original-medicare/appeals-level-1-company-handling-medicare-claims-redetermination
- ↑ https://www.medicare.gov/claims-appeals/your-right-to-a-fast-appeal
- ↑ https://www.shiptacenter.org/about-us/
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/can-someone-file-an-appeal-for-me
- ↑ https://www.medicare.gov/claims-and-appeals/file-an-appeal/appeals.html
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/filing-an-appeal-if-i-have-original-medicare/appeals-level-1-company-handling-medicare-claims-redetermination
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/filing-an-appeal-if-i-have-original-medicare/appeals-level-1-company-handling-medicare-claims-redetermination
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/filing-an-appeal-if-i-have-original-medicare/appeals-level-1-company-handling-medicare-claims-redetermination
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/medicare-prescription-drug-coverage-appeals/appeals-level-2-reconsideration-by-independent-review-entity
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/medicare-prescription-drug-coverage-appeals/appeals-level-2-reconsideration-by-independent-review-entity
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/medicare-prescription-drug-coverage-appeals/appeals-level-2-reconsideration-by-independent-review-entity
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/filing-an-appeal-if-i-have-original-medicare/appeals-level-3-hearing-before-administrative-law-judge
- ↑ http://www.hhs.gov/omha/Coverage%20and%20Claims%20Appeals/Request%20an%20ALJ%20Hearing/request_hearing.html
- ↑ http://www.hhs.gov/omha/Coverage%20and%20Claims%20Appeals/Request%20an%20ALJ%20Hearing/request_hearing.html#
- ↑ http://www.hhs.gov/omha/Coverage%20and%20Claims%20Appeals/Request%20an%20ALJ%20Hearing/request_hearing.html#
- ↑ http://www.hhs.gov/omha/Coverage%20and%20Claims%20Appeals/Request%20an%20ALJ%20Hearing/request_hearing.html
- ↑ http://www.hhs.gov/omha/Coverage%20and%20Claims%20Appeals/Request%20an%20ALJ%20Hearing/request_hearing.html
- ↑ http://www.hhs.gov/omha/Coverage%20and%20Claims%20Appeals/Request%20an%20ALJ%20Hearing/request_hearing.html
- ↑ http://www.hhs.gov/omha/Coverage%20and%20Claims%20Appeals/Your%20ALJ%20Hearing/hearing.html
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/filing-an-appeal-if-i-have-original-medicare/appeals-level-3-hearing-before-administrative-law-judge
- ↑ http://www.hhs.gov/dab/divisions/dab101.pdf
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/appeals-level-4-review-by-medicare-appeals-council
- ↑ http://www.hhs.gov/dab/divisions/dab101.pdf
- ↑ http://www.hhs.gov/dab/divisions/dab101.pdf
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/appeals-level-4-review-by-medicare-appeals-council
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/appeals-level-5-federal-district-court-judicial-review
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/appeals-level-5-federal-district-court-judicial-review
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/medicare-prescription-drug-coverage-appeals
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/medicare-prescription-drug-coverage-appeals
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/medicare-prescription-drug-coverage-appeals/drug-plan-appeals-level-1-redetermination-from-your-drug-plan
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/medicare-prescription-drug-coverage-appeals/appeals-level-2-reconsideration-by-independent-review-entity
- ↑ https://www.medicare.gov/claims-appeals/file-an-appeal/medicare-prescription-drug-coverage-appeals/appeals-level-2-reconsideration-by-independent-review-entity
- ↑ https://www.cms.gov/Medicare/Appeals-and-Grievances/MedPrescriptDrugApplGriev/Downloads/Flowchart-Medicare-Part-D.pdf